Keratoconus
What is Keratoconus?
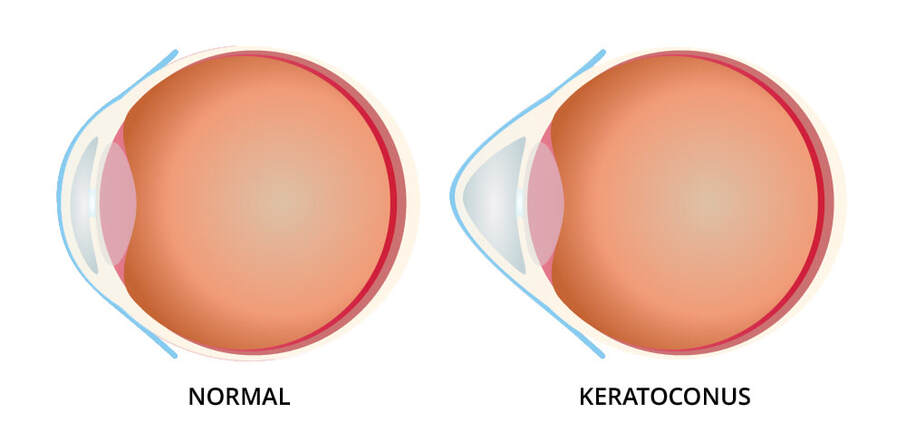
Keratoconus is a condition that affects our cornea (the clear membrane at the front of the eye). The cornea is supposed to have a smooth regular shape and is responsible for focusing light on the retina.
In patients with keratoconus, the cornea begins to progressively become thinner usually between the late teens and early twenties. This thinning causes the cornea to protrude in the centre and assume a conical irregular shape.
Keratoconus usually involves both eyes, but one eye may be more advanced than the other.
Symptoms of Keratoconus
- Blurred vision
- Ghosting of images
- Distorted vision
- Sensitivity to light
- Glare
- Frequent change in glass prescriptions
Causes of Keratoconus
Various genetic and environmental factors contribute to it.
Known risk factors include a family history, a tendency towards eye rubbing, history of asthma or frequent allergies and other conditions like Downs Syndrome and Ehler Danlos Syndrome.
How do you diagnose Keratoconus?
If you have the above symptoms, or if you have recently been diagnosed with corneal astigmatism and are not comfortable with your glasses, a visit to the ophthalmologist is a must.
After testing your power, you will be examined under the slit lamp biomicroscope. If there is a strong suspicion of keratoconus you will be advised a corneal scan, called a corneal topography, which maps out the thickness and shape of your cornea.
There are various types of scans to map the same, some which act as a screening tool, and others that aid in deciding further management.
Once diagnosed, how is Keratoconus managed ?
You will be first graded according to the severity of the disease- this takes both thickness and corneal steepening into account.
For mild cases, with a good corneal thickness and no significant steepening, we tend to observe the progression of the disease. This requires serial corneal topographies 3-6 months apart.
Moderately severe cases with thin corneas are managed with a therapeutic procedure called corneal collagen cross linking (CXL or C3R) which uses ultraviolet light and a chemical called riboflavin to arrest corneal thinning and halt the progression of the disease.
Cross linking may be accompanied with the insertion of corneal ring segments – INTACS made of a polymer or CAIRS made of donor corneal stromal tissue. These ring segments serve to flatten the cornea and augment corneal thickness.
Very severe cases may need a partial corneal transplant called DALK where the anterior corneal layers are removed and replaced with donor tissue.
FAQ
Is cross linking a laser procedure?
Cross linking is merely a therapeutic procedure to prevent the cornea from thinning out further. It is not a laser procedure to remove glasses. You will still require glasses post procedure, though the final refraction value will be arrived at 6 months post procedure. Prior to that, temporary glasses may be used.
What is the role of contact lenses?
Contact lenses sit directly on the corneal surface, and there are various types of these lenses that have been proven beneficial in keratoconus as they regularise the shape of the cornea and flatten a steep curvature. This improves quality of vision. Before prescribing lenses, you will undergo a contact lens trial so you are prescribed lenses appropriate to your stage of the disease.
Will Keratoconus make me blind?
Keratoconus, if diagnosed early and managed appropriately, will NOT make you blind. It is not curable, but can certainly be amended.
There is a sight threatening complication of advanced untreated keratoconus called acute hydrops, in which the cornea becomes so thin, that the fluid inside the eye called aqueous breaches its barrier and flows into the corneal layers, making the cornea opaque, oedematous and boggy. This too can be managed, however it is advisable to get treated before this happens if you already know that you have this condition.
In conclusion, it is prudent to remember that any condition can be endured once treated early and appropriately. Regular follow up and dedication from a patients’ side is essential with some basic knowledge of the condition which helps in setting realistic expectations.